Dr. Kim and colleagues recently published “Outcomes After Elevation of Serratus Anterior Fascia During Prosthetic Breast Reconstruction” in the Annals of Plastic Surgery. Immediate prosthetic breast reconstruction is becoming increasingly popular; this approach often involves the placement of an implant below the pectoralis muscle1. Although the inferolateral border of the prosthetic may not be covered which may cause rippling, contour deformities, migration etc2. To create more support for the implant, some surgeons turn to ADM, muscle flaps, or elevating the serratus muscle, which is located in close proximity to the pectoralis muscle1,2. ADM is still a relatively new technology and there is not a consensus if the potential risks outweigh the financial burden1,2. Using autologous tissue like a muscle flap or the proximal serratus muscle may lead to post-operative pain or there may be residual defects in the muscle’s ability to function after surgery1,3. In order to understand why the location of the serratus anterior is ideal for supporting the inferior portion of the prosthetic device and consider what the kinetic defects may be post surgery it’s prudent to consider the anatomy and action of the key muscles involved. Although, Dr. Kim thinks it is crucial to keep in mind that every patient will have an individual course of treatment and that it is important to make the decisions about your breast reconstruction that best fits your needs.
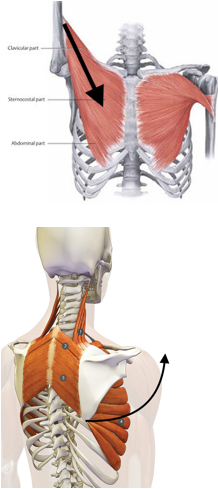
The pectoralis major muscle is a thick fan-shaped muscle located deep to the breast tissue4.
Directly deep to the pectoralis major muscle is the pectoralis minor muscle4. Deep to the pectoralis minor, a feather like muscle covers each rib called the serratus anterior muscle4. If these feather-like muscles are elevated off of the ribs they can act almost like a flower box hanging off the side of a wall supporting the implant inferiorly. If the thin connective tissue casing the fascia is disrupted instead, it can perform the same supportive task as the muscle except being a more pliable material and won’t have the same effect on altering the patient’s capacity movement.
The serratus muscle assists in upward rotation of the arm working in opposition to the pectoralis muscle that draws the arm inward (adduction)4. Although these muscle appear to have fibers running in the same direction they cause a very different result because of the difference in insertion point4. The serratus muscle inserts on the scapula, shoulder blade; when this muscle shortens it sends the arm overhead4. Whereas the pectoralis muscle inserts on to the humerus (arm) and when it shortens it brings the arm back towards the body4. During subpectoral breast implant placement, manipulation is required of the pectoralis muscle and may lead to some weakness or loss of function4. In the method that elevates the serratus anterior fascia described by Dr. John Kim and colleagues there is a movement of structures but not a severing.
In order to study the utility of this technique a retrospective chart review was performed examining patients who underwent the procedure with the elevation of the serratus muscle or fascia. They concluded that elevation of the serratus fascia is a safe and viable alternative to the disruption of the muscle and use of ADM. If you are considering undergoing breast reconstruction at Northwestern Medical Group, speak with Dr. John Kim about what method (ADM, muscle flap, or elevation of the serratus muscle or fascia) will offer you the best coverage and the best result.
1. Seth, A. K., Hirsch, E. M., Kim, J. Y., & Fine, N. A. (2017). Outcomes After Elevation of Serratus Anterior Fascia During Prosthetic Breast Reconstruction. Annals of Plastic Surgery.
2. Lee, J. H., Park, Y., Choi, K. W., Chung, K. J., Kim, T. G., & Kim, Y. H. (2016). The Effect of Sterile Acellular Dermal Matrix Use on Complication Rates in Implant-Based Immediate Breast Reconstructions. Archives of Plastic Surgery, 43(6), 523-528.
3. Saint-Cyr M, Dauwe P, Wong C, et al. Use of the serratus anterior fascia flap for expander coverage in breast reconstruction. Plast Reconstr Surg. 2010;125: 1057–1064.
4. Gray, Henry. Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918; Bartleby.com, 2000. bartleby.com/107/.
5. http://www.top.me/wp-content/uploads/2014/06/kettlebell-swing.jpg
7. https://s-media-cache-ak0.pinimg.com/originals/45/ca/e3/45cae3d3f9ccfc6e36f0cf0a48998b78.jpg
