During the normal course of aging, post pregnancy, or after massive weight loss, the tissues that make up the breast can become more lax. Dr. John Kim says that women who are a candidate for a breast lift are those who are happy with their breast volume but are unhappy with their sagging appearance. Breast tissue is located within the deep fatty layer immediately behind scarpa’s fascia; the upper part of the breast is held to the chest wall by Cooper’s ligaments and the lower part of the breast is attached to fascia within the submammary fold (Frame 2017). Breast laxity is dependent on: volume, consistency of tissues, skin compliance, genetics, and the skeletal frame (Frame 2017).
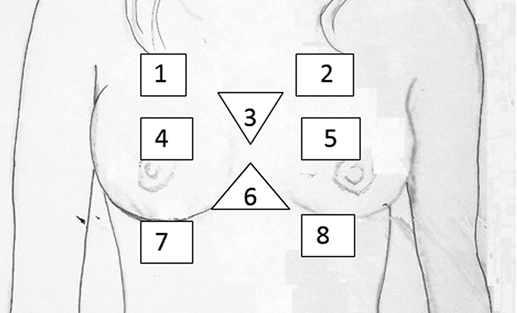
The skeleton is the frame that holds muscles and soft tissue, which then create the frame that the skin and breast tissue drape over. The visual appearance of the breast is dependent on the shaped and distribution of the aforementioned tissues. Frame et. al defined the breast based on 8 separate units, inspired by the 8 gluteal aesthetic units defined by Dr. Centeno in a 2015 paper published in the Aesthetic Surgery Journey. These 8 points are places of measurement and symmetry: 1 and 2, 4 and 5, 3 and 6, as well as 7 and 8. Noting asymmetry in points 1 and 2 may suggest irregular pectoralis major muscle insertion point. A sunken appearance in units 4 and 5 can present the breasts as being smaller than they are. The volume of 3 and 6 should be small to create a narrow cleavage. Units 7 and 8 want to be seen versus covered by ptotic, sagging, breasts.
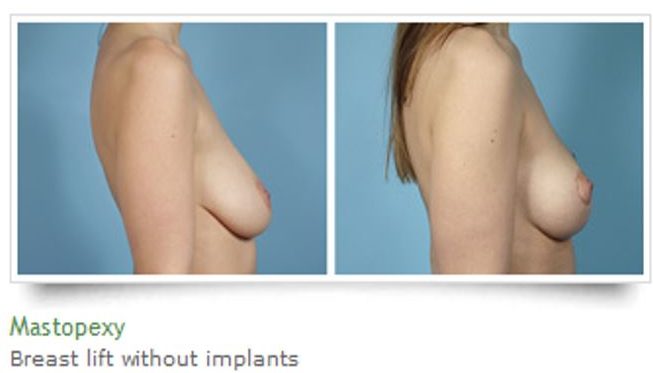
Women have a number of options to decide how they want to proceed with a breast lift or mastopexy. In an article published in the Aesthetic Plastic Surgery Journal de Bruijn describes the mastopexy as a procedure that “counteracts the adverse effects of gravity and decrease in skin elasticity and firmness of the female breast.” In order to create a method for surgeons to create reliable long lasting results scientists created a 3-D woven mesh which creates an internal bra which becomes incorporated into breast tissue (de Bruijn).
The ideal internal bra will: not interfere with mammography, allow for long term host tissue replacement, and maintain strength, easy for the surgeon to use, easily stored, available in varying sizes, affordable, natural feel (Baxter). There are different internal bra materials available including: polypropylene mesh, human derived ADM, porcine derived ADM, and SERI scaffold. Polypropylene mesh is durable, affordable and available in varying sizes and shapes; but it is a foreign body and as such may lead to infections or exposure, in addition they may interfere with mammograms (Baxter). Both human derived and porcine derived ADM are potentially very long lasting, but they are expensive, limited in their size options, and there is a potential for the need for a long term drain, seroma development, and red breast syndrome (Baxter). Human derived ADM is more elastic than porcine-derived ADM, although porcine-derived ADM provide instant thickness (Baxter). Compared to the other materials there is very limited clinical data for SERI scaffold, but it is very affordable, come in varying sizes, and they may have some advantages because of their open weave material which can facilitate fluid dissipation and mesh integration (Baxter).
If you are interested in having a breast lift procedure come and speak with Dr. John Kim at Northwestern Medical Group. To see more photos of patients who have undergone this procedure click here.
Baxter, R. A., Khan, U. D., Watson, H. K., Purnell Traverso, L. C., Mastella, D., Wollstein, R., & Mommaerts, M. Y. Internal bra: a unifying solution for reconstructive and aesthetic breast surgery issues.
de Bruijn, H. P., & Johannes, S. (2008). Mastopexy with 3D preshaped mesh for long-term results: development of the internal bra system. Aesthetic plastic surgery, 32(5), 757-765.
Frame, J. (2017). The waterfall effect in breast augmentation. Gland Surgery, 6(2), 193.
Frame JD, Connolly C. Framing the Breast. Aesthet Surg J 2015;35:NP106-12. 10.1093/asj/sju088